Practical Nursing Program Hands on Learning For Real World Impact
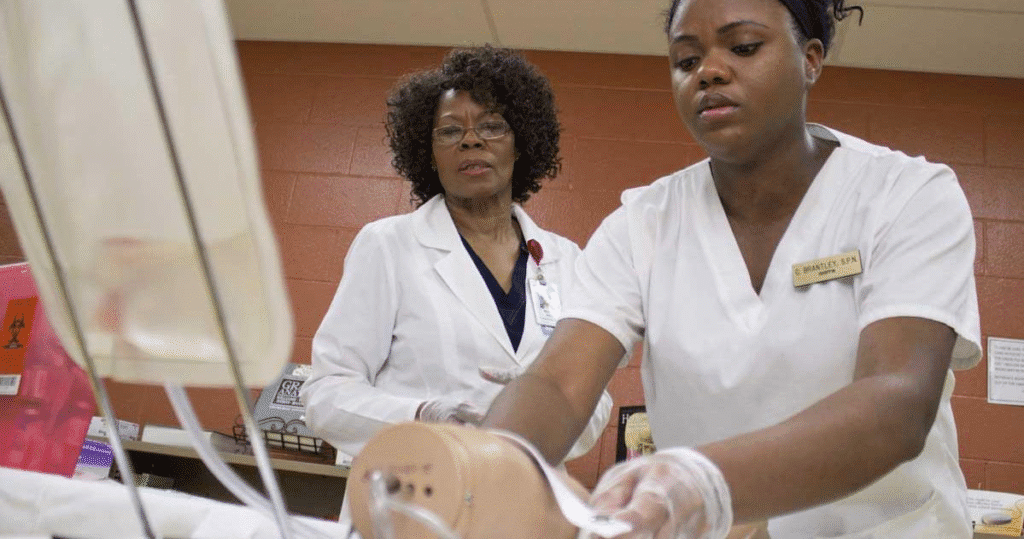
The healthcare industry today continues to seek skilled and caring nurses, leading to an acute need for individuals who can provide quality nursing care.The Practical Nursing Program represents a line of study for persons wishing to develop a nursing career that is an efficient, hands-on approach to obtaining education and experience. This type of program also must create a tie between the advanced classroom theory and the real clinical experience you will gain from the clinical practice, while giving students and aspiring nurses the knowledge, skills and attitude to be competent and confident to make a positive impact on the individual lives of patients. Experiential education is game-changing for preparing nursing students for real life practice in health care. It develops critical thinking, fosters empathy, and develops technical skill. Through simulated labs, monitored clinical experiences, and an interactive curriculum, students develop both the knowledge and the practical skills to thrive in any clinical environment. Building a strong foundation through applied education A vital element of the Practical Nursing Program is its emphasis on creating a solid foundation in the foundational principles of healthcare through applied education. Nursing students are introduced to a variety of essential concepts of nursing, such as anatomy, physiology, pharmacology, and patient care techniques. However, instead of having the student learn entirely in the classroom — the Practical Nursing Program places the classroom elements into practice through clinical experiences. This provides the nursing student with the opportunity to visualize how nursing concepts occur in real-life clinical cases. The collision of knowledge and experience ensures that practical nursing learners develop knowledge and competency. Clinical training The emphasis of the Practical Nursing program is clinical practice which provides the students the opportunity to gain supervised experience in hospitals, long-term care facilities, and other health care settings. By means of practical experience, students will learn about their responsibilities caring for patients, communicating with other health care professionals, and adjusting to the rapid pace of learning in the clinical environment. Greater awareness and understanding of different medical conditions as well as human feelings will result from their experiences with real patients. Developing professional and interpersonal skills The Practical Nursing Program is centered on the development of professional and interpersonal skills. Students are educated to communicate effectively with patients, families and members of the health care team. They are shown how to listen with empathy, provide support, and communicate their message in a way that is uncomplicated and clear. Each of these demonstrates critical communication skills an individual needs to build trust, as well as provide safe, quality nursing care. Professionalism is important in nursing education as students learn the ways in which to work collaboratively on an interprofessional team, develop leadership skills, and think in ethical ways. Students practice professionalism in their work by maintaining confidentiality, recognizing cultural similarities and differences, and advocating for the best interest of the patient. Simulation labs: Preparing for real-world scenarios Simulation laboratories create an experience that reflects a hospital setting and provide nursing students with a safe place to complete nursing skills. Nursing students can perform things such as wound care, catheter insertions, or emergency procedures using simulation scenarios. Simulation training provides an excellent opportunity for nursing students to build muscle memory for procedures they will eventually perform, as well as simulating what it feels like to remain calm, cool, and collected while in a stressful situation. Students are also given an opportunity to be comfortable making mistakes within the practice environment as mistakes are a part of learning. Critical thinking and decision-making in nursing practice The practical nursing program builds upon technical skills and develops critical thinking and good judgment. Nurses make decisions every day that impact patient outcomes. The program offers case studies, problem-based learning, and patient situations that require students to evaluate situations and respond in real time to develop thinking skills. In this way, the process allows students to evaluate symptoms, utilize data, and prioritize care in an efficient way. They will use both logic, empathy, and clinical thinking in every encounter Bridging the gap between education and employment An important advantage of the practical nursing program is that it can link education to employment because graduates are able to enter the workforce as soon as they finish the program. The practical nursing program hybrid model with classroom learning, a clinical placement and simulation labs prepares students in the qualities business is looking for when hiring in health care settings. The program teaches clinical skills and provides an understanding of workplace environments, documentation, and healthcare policies. The lasting impact of hands-on learning Experiential learning enhances nursing students’ attitudes to care deeply while creating a sense of fulfillment and motivation. Seeing the positive impacts of their own care ensures students understand the innate value of their roles. The emotional impact promotes engagement with nursing and enhances ongoing learning and development. Conclusion The practical nursing program prepares students for a rewarding life where they are knowledgeable, caring, and committed to serving others. With a focus on practical learning, graduates will learn and be confident to affect change in practice. Students gain the knowledge and competence to respond to a changing healthcare environment with care and expertise through clinical experiences, simulations and other methods of education.
Accelerated Practical Nursing Program Fast Track Your Future

The healthcare sector is one of the fastest-growing fields in the world, and the demand for qualified healthcare workers who have the education, training, and desire to provide compassionate and competent care to patients has never been greater. Licensed Practical Nurse (LPN) is one of the most significant professions in healthcare. LPNs are an important member of the healthcare team in hospitals, clinics, long-term care facilities, and community health. The accelerated practical nursing program allows students who are highly motivated to achieve licensure in less time by gaining the education and knowledge necessary to become employed. While the traditional educational path of practical nursing programs usually takes several years, accelerated programs generally employ a rigorous and intensive schedule to combine coursework, clinical experience, and professional preparation. Understanding the structure of accelerated practical nursing programs Accelerated practical nursing programs are developed to fit a traditional curriculum into a shortened period yet not cutting short the skill and knowledge attainment. Students should expect a more in-depth course of study, with classes, labs, and clinical rotations scheduled into shorter periods of time. This allows students to receive the same core education as those in traditional programs, covering all the necessary anatomy, physiology, pharmacology, and fundamentals of nursing courses. In addition to class time, students in the accelerated nursing programs practice hands-on learning in clinical training. Students are supervised by qualified instructors and practice direct patient care in real-world health care settings. This balance of lecture education and hands-on clinical training supports adequate education in theory, as well as confidence in performing the essential duties of nursing with a real-life patient. Benefits of choosing an accelerated nursing path A primary advantage of accelerated practical nursing programs is the possibility of a quick entry into the workforce. Rather than waiting two or three years to begin a career, graduates of an accelerated program typically can finish their course work anywhere from one academic year to eighteen months, depending upon the program. Therefore, these programs appeal to people who have a desire for employment and financial stability without having to wait for several years to pursue a job. Another advantage of an accelerated practical nursing program is the compact learning approach. Because this type of program is shortened, students are engaged directly in nursing education on a daily basis which frequently helps confidence retention of learning and the development of practiced skills. The consistent involvement of the students transforms into a solid foundation of knowledge and skills that provide the students with the skill set required as a licensed practicing nurse and for practical nursing in the care of patients. Choosing the accelerated program path ultimately reflects the urgent care shortage of nurses in today’s healthcare system. Students attending an accelerated program begin with an associate of science degree with an educational mindset that seeks out employment that is abundant and valuable reciprocally. There is always a pressing need for competent individuals in hospitals, clinics, and long-term care facilities and both current students and associates, typically find themselves entering into a future health career with an abundance of opportunity. Long-term career opportunities An accelerated practical nursing program is not only a fast track into the healthcare field but also a pathway to long-term career potential. A Licensed Practical Nurse can work in a variety of settings, from hospitals to private practices, and often a licensed practical nurse will later continue education and enroll in a bridge program to attain Registered Nurse (RN) status or a higher degree in nursing. The prep work from working through an accelerated program enables graduates to build experiences toward future careers and their professional development pathways. Graduates can either continue to do direct patient work or transition into a specialty area, taking with them the skills, discipline, and flexibility gained from the intensive education of a fast track nursing program. Meeting the needs of modern healthcare Contemporary healthcare systems depend on competent personnel who are responsive to patient needs in a timely manner. Accelerated practical nursing programs contribute to this demand by training competent graduates in a more timely manner. Because healthcare organizations are facing nursing shortages, the accelerated route is a timely solution for both students expecting a career and employers expecting necessary staff. This alignment of the educational process and the workforce demand is part of the reason accelerated programs have realized popularity. By balancing speed and quality, accelerated programs ensure that the healthcare system has a steady stream of qualified nurses contributing to the workforce. Conclusion Healthcare systems often depend on qualified people to respond rapidly to customer service needs. Accelerated practical nursing programs fill this demand by preparing capable graduates in a significantly shorter time. This offers an immediate solution to nursing staff shortages experienced by healthcare facilities and assists students, as soon-to-be graduates, in pursuing a desired career. The alignment between education and workforce demand is certainly part of the growth of accelerated programs. Education that combines speed with quality assures the healthcare system that qualified and competent nurses continue to enter the workforce to become productive members of the service arena.
What Jobs Can You Get With A Practical Nursing Certificate?

The healthcare industry continues to grow at an increasing pace creating an ongoing need for each level of qualified staff enabling safe care to be provided. One of the quickest and least stressful ways to enter healthcare is a practical nursing certificate, allowing a person to enter health care without the time and financial commitment of a registered nursing (RN) program. Practical nursing programs are usually 12-18 months and provide a student with the clinical and theoretical knowledge required to be either a Licensed Practical Nurse (LPN) or a Licensed Vocational Nurse (LVN)” but depends on what state they reside in. Practical Nurses are important not only to the day to day operations of a healthcare practice, but are essential for positive patient care outcomes.When the practical nursing certificate is awarded, and when the NCLEX-PN licensing exam is passed, a new graduates credentials can be used to start searching for employment opportunities in a hospital, clinic, long term care, a home health or school setting. Become a licensed practical nurse (LPN) For completing the Practical Nursing program, the common and most direct outcome is to become a Licensed Practical Nurse (LPN), or in some states, a Licensed Vocational Nurse (LVN). LPNs provide care in healthcare settings, under the supervision of Registered Nurses (RNs) and Physicians. LPNs provide certain components of nursing care, including: Monitoring a patient’s health status by taking vital signs (blood pressure, pulse, respiration, temperature). Administering medications and injections that are prescribed. Assisting patients with activities of daily living (bathing, dressing, eating). Basic care of wounds and putting on dressings. Informing other nursing teams members of changes in a patient’s status. LPNs help to maintain quality of care; LPNs assist with both physical supportive actions and emotional supportive actions throughout the continuum of care process. Work in a variety of healthcare settings Home health nurse As the need for home-based care continues to increase, many LPNs choose to work as home health nurses. In this role, practical nurses would make visits to patients’ homes to provide care including dressing of wounds, giving medications, or overseeing progress in health. Home health nurses are independent workers and must be capable of making sound decisions and be motivated. A home health nurse often has a more flexible schedule, and the opportunity to incorporate long relationships with patients, similar to chronic conditions or patients recovering from surgery. Rehabilitation centers Rehabilitation Centers provide LPNs a chance to work with patients recovering from serious sickness, injuries, or disorders. When the LPN is a rehabilitation nurse, they help the client become independent again so that they may return to their daily life. Rehabilitative LPNs often assist in physical therapy (PT) exercises, pain management, medication administration and education. Rehabilitative care is a great fit for LPNs who want to play an active role in a patient’s healing process. Hospice care Hospice is another area where practical nurses can have a big impact. LPNs in hospice care may manage pain, administer medications, provide emotional support to families and provide comfort to the patient during their final days. Working as an LPN in hospice care requires emotional strength, compassion, communication skills, but it can be very rewarding for many practical nurses. Pediatric LPN Become a pediatric LPN if you enjoy working with children. Pediatric practical nurses generally work in clinics, hospitals, or a pediatrician’s office providing care to infants, children and adolescents. You may provide vaccinations, growth checks, and education to parents. This role requires gentleness, patience, and a child-friendly approach. Additional pediatric credentials and certifications could improve job opportunities. Specialize in a niche area of care LPNs can provide care for specialization in the following areas: Pediatrics – working with young patients in pediatric clinics, pediatric hospitals, or long-term care facilities. Geriatrics – working with older patients with age related health conditions. Hospice and palliative care – providing comfort and care for patients who are nearing the end of life, while ensuring comfort and quality of life. Maternity and obstetrics – involving working with women during the prenatal period, the labor and delivery phase, and immediately after the woman delivers her baby. Surgical nursing – preparing patients and assisting the physician through surgical procedures. These specialties allow LPNs to work in the field of their choosing, but these specialties may also provide access to higher paying positions and leadership positions in the area of their choosing. Opportunities for leadership and mentoring In a practice setting, senior LPNs typically assume leadership roles. As an example, they may function as Charge Nurses, directing a group of nursing assistants and LPNs. They may take on new nurses as their mentees, training them and advising them during their transition into practice. This is how LPNs can impact the work culture of their practice environment and quality of patient care.
When Was The First School Of Practical Nursing In The United States Founded?

The history of nursing education in the United States has reflected the development of the United States toward a more organized, equitable, and competent healthcare system. The healthcare landscape began to change as the 19th century gave way to the 20th century, in part due to the industrialization and urbanization of America, which included technological advancements in medicine. New hospitals were being built in order to treat patients with complex and growing needs. While reserved nurses play an important role in the health care team, it was not uncommon for people to be without or short of nursing services, especially in rural areas and poorly economically supported urban areas. In essence, practical nurses were developed to meet the needs of organized, available, and competent health care workers. In this regard, practical nursing developed a course of training to provide people, primarily from working-class backgrounds, the necessary skills to be able to assist physicians and registered nurses in the care of patients. The founding of the first practical nursing school The first school of practical nursing in the United States was founded in 1892 in Brooklyn, New York. Known as the Ballard School, the school was established under the Young Women’s Christian Association (YWCA). During a time when formal education was limited for women, and especially for women in science or medicine, the Ballard School provided a formal and organized educational program, which included actual classroom instruction, and trained women to provide basic nursing care for patients. Evolution from home care to professional training The original intent of the program was to train home caregivers, but the program quickly moved toward preparing professional training of nursing aides for hospitals and health care in the community. The Ballard School offered a progressive curriculum at the time that lasted approximately three months and included education on basic anatomy and physiology, sanitation, nutrition, and personal care. Students could also take part in practical hands-on training that allowed them to learn how to assist with bathing, feeding, and observing patients. Key values and teaching philosophy ams The Ballard School provided information focusing heavily on cleanliness, ethics, and observation, key aspects of nursing education today. While the offerings of the Ballard School were more limited than those of a registered nurse, the knowledge and training that it offered its graduates allowed them to contribute in both hospital and home settings. Accessibility and social impact The Ballard School was notable for its commitment to accessibility in education. Creating short-term, skills-focused training, it enabled women from lower socioeconomic backgrounds to gain a credential in the healthcare profession over a short time span, thus providing a level of democratization of nursing education. Many women benefited financially and gained independence, and many underserved communities received additional standards of care. Influence and expansion of practical nursing education The success of the Ballard School inspired other schools across the country and their variations of practical nursing that met the health discrepancies where they were located. Over the decades ahead, practical nursing continued to be popular and in demand. The economic repercussions of the Great Depression, and the healthcare demands of World I and World II, placed more stress on hospitals in search of capable staff who could work at a low cost. In this context, practical nurses were viewed increasingly as a vital resource, providing high-quality care for lesser compensation than the subsequent tier of the nursing pyramid—registered nurses. Accordingly, this period of focus and attention resulted in an exceptional increase in the sheer number and size of practical nursing education programs, many of which were developed in collaboration with local hospitals and/or public health departments. Formation of national standards The National Association for Practical Nurse Education and Service (NAPNES) was created in 1947 with a focus on developing standards and supporting the practical nurse profession. One of NAPNES’s first achievements was the development of a national curriculum and promotion of credentials which resulted in the use of the professional titles of Licensed Practical Nurse (LPN) and Licensed Vocational Nurse (LVN) depending on the jurisdiction, becoming institutionalized. The licensure formally recognized the practice of practical nursing with examinations, licensing, regulatory oversight, and requirements for continuing education. Establishing a tiered nursing structure The development of the Ballard School and subsequent LPN programs created a tiered structure for nursing in the United States, which enabled levels of variation in the training, responsibility, and pay of healthcare careers that simply did not exist previously. This variation created a pathway to expand access to healthcare professions: people can now choose from varied levels of education and credentials over the course of their lifetime. Many LPNs went on to become Registered Nurses (RNs), but those that did not, specialize in areas of practice, such as geriatrics, pediatrics, or home health, which were not as easily available to them previously. Modern-day practical nursing programs Today, practical nursing programs are offered by vocational schools, community colleges, and in some high schools across the country, and training programs run from about 12 to 18 months in duration. Along with technology and healthcare delivery changes, the same core values established by the original Ballard School remain in place: continued access, hands-on education, value for patient-centered care, and continued access to try to empower people, especially women, by access to education and career opportunities. Lasting legacy of the ballard school The impact of the Ballard School continues to be commemorated today, not only as the origin of practical nursing education in the U.S. but as part of a legacy of public health progress and gender equity. The effects, emanating from such a simple institution, have continued to extend far beyond Brooklyn, affecting the lives of millions of patients and the beginnings of countless nurses. By institutionalizing practical nursing, the Ballard School initiated a system of more available and efficient healthcare parameters for the 20th century and beyond.
What Is A Graduate Certificate In Nursing?

In the dynamic healthcare environment, the need for highly qualified nursing professionals has never been higher. With the increased complexity of patient care and innovative technologies that are being introduced, nurses are expected to upgrade their skills and respond to specialized positions within the healthcare framework. This is where a Graduate Certificate in Nursing steps in—a concentrated, advanced degree program for registered nurses (RNs) looking to enhance their proficiency, extend their employment opportunities, or switch over to leadership or specialized roles. In contrast to a full master’s degree, which involves a more extensive commitment, a graduate certificate is a shorter, focused route for nurses to acquire new skills and credentials in a specialized practice area. A Graduate Certificate in Nursing fills the space between undergraduate education and a master’s or doctoral degree, providing a chance for professional development and career advancement. Whether a nurse wishes to become specialized in clinical leadership, critical care, mental health, or education, a graduate certificate gives them the theoretical knowledge and practical skills necessary for success. It is also used as a stepping stone for those thinking of further postgraduate study in the future. Graduate certificate in nursing A Graduate Certificate in Nursing is a postgraduate academic degree program aimed at registered nurses who have finished their bachelor’s degrees (usually a Bachelor of Science in Nursing or its equivalent). The certificate enables nurses to specialize in a particular field of nursing practice without enrolling in a full master’s degree program. It usually includes 3–5 specialized courses, on theoretical and practical topics specific to the area of interest, like leadership, clinical practice, or education. This specialized study allows nurses to expand on their current clinical skill, use evidence-based interventions, and remain current on healthcare trends. Graduate certificates tend to be sought by nurses who want to specialize in a specific field, for example, acute care, perioperative nursing, mental health, or palliative care, or work in higher-level roles such as clinical educators or nurse managers. The length of a graduate certificate program is typically between six months and one year part-time, but it can differ based on the organization and mode of study. Key benefits of a graduate certificate in nursing One of the most significant benefits of earning a Graduate Certificate in Nursing is career advancement. With the healthcare sector becoming more and more specialized, employers are looking for nurses with specialized qualifications to undertake advanced clinical jobs or leadership positions. The graduate certificate signifies the dedication of a nurse to continuing education, and this can become a key to upper-level jobs, greater responsibilities, and improved salary opportunities. A further advantage is the convenience of the program. Most graduate certificates are geared towards working professionals, with distance learning or hybrid learning opportunities to fit around nurses’ full-time workloads. This is how nurses can remain at work while completing their studies, enabling them to immediately transfer new skills to their actual clinical practice. A graduate certificate also serves to give nurses confidence to practice in a specialized area of care so that they are able to deliver evidence-based interventions and make deliberate decisions that will improve patient outcomes. Also, for those looking to enter the master’s degree in nursing (MSN), a graduate certificate will typically enable credits to be transferred, saving time and expense on a future postgraduate program. Common specializations in graduate nursing certificates Graduate nursing certificates usually specialize in a particular area of clinical or professional practice. Among the most common specializations are: Clinical leadership: This specialization is intended for nurses who want to enter leadership positions. It is centered on management competencies, healthcare systems, quality improvement, and team dynamics. It prepares the nurses to manage teams, direct clinical operations, and implement evidence-based policies. Acute care nursing: This specialty provides nurses with superior knowledge and skills to care for critically ill patients, typically in environments such as emergency departments or intensive care units (ICUs). Mental health nursing: Mental health specialization enables nurses to care for patients with mental illness, learn about psychological treatments, and function within multidisciplinary teams to provide whole-person care. Palliative care: Nurses here are taught to cope with the complex needs of terminally ill patients, addressing pain, emotional support, and end-of-life care. Nursing education: This program is geared towards curriculum design, teaching techniques, and test-taking skills to equip nurses to become teachers in academic or clinical environments. These specializations reflect the diverse opportunities within nursing, allowing professionals to align their studies with their career interests and the healthcare needs of their communities. Entry requirements and application process To enroll in a Graduate Certificate in Nursing, applicants must typically hold a current nursing registration in their country of practice and have completed an undergraduate nursing degree such as a Bachelor of Science in Nursing (BSN). The programs might demand a minimum number of clinical hours in the specialized area, especially for specializations such as critical care or perioperative nursing. The application process typically includes submission of an online application using the institution’s admissions website, academic transcripts, a resume, and sometimes a statement of purpose outlining the reason for pursuing the certificate. Letters of recommendation or proof of current professional registration may be asked for in some programs. For students from overseas or non-English-speaking countries, English language proficiency (e.g., IELTS or TOEFL test scores) will also be required. It is best to check each program’s entry requirements prior to application. Career outcomes after completing a graduate certificate in nursing A Graduate Certificate in Nursing adds to the qualifications of a nurse and can open up opportunities for career advancement in many different settings. Graduates can advance to senior positions like nurse educator, nurse manager, care coordinator, or clinical nurse specialist based on their area of specialization. For instance, a graduate with a certificate in critical care may be suited for leadership positions within an ICU, whereas a graduate with a certificate in nursing education may adopt teaching roles in academic organizations or healthcare establishments. The further expertise from a graduate certificate also renders
How To Get A Nursing Transcript Certificate?

In the healthcare field, record-keeping of academic progress is a professional development and future opportunity process. One important document is the nursing transcript certificate. A nursing transcript is a document that shows a student’s academic progress within the nursing program, including course completion, grading basis, grades achieved, and completed credits. You will need an accurate and up-to-date nursing transcript certificate if you are pursuing your first nursing license, advancing your education, or exploring opportunities abroad. Many nurses may not know how or where to get a transcript, particularly if they graduated or went to school some years ago, or because of the institution’s process. This may seem intimidating at first since there are often several steps involved in the transcript process, including official requests, verification, and, in some situations, the stress of seeking accountability for the paperwork and record-keeping methods of an institution or bureaucracy. Nonetheless, once you are clear on the process, it will be much easier to secure yourself a nursing transcript certificate. Understanding the importance of a nursing transcript certificate A nursing transcript certificate is an official document that truly represents your academic experience and accomplishments. It offers extensive details on courses completed, grades obtained, and credits earned. This report is commonly requested when requesting nursing licensure or registration from another state or country, requesting admission to advanced education programs like a Bachelor of Science in Nursing (BSN), Master of Science in Nursing (MSN), or Doctorate in Nursing Practice (DNP), job application where the employers have to confirm your nursing education, or for credential assessments for immigration. Without an authentic transcript, your educational credentials will not be honored, and your career will be hindered. This is why it is important to have an official and current nursing transcript certificate when required. Identifying the issuing authority The process of getting your nursing transcript begins by seeking the authority issuing the transcript. This will, in most instances, be the nursing school, college, or university you attended for your nursing course. For example, if you graduated with a Bachelor of Science in Nursing (BSN) degree from a certain university, you should get in touch with the registrar or records office of that university. In the case of diploma or certificate courses, e.g., those in the Philippines, the authority where the degree is issued could be the school of nursing or the attached examination board. Preparing the required documents It is important to secure all documents before requesting a nursing transcript certificate. Requirements can differ based on the institution or country, but standard documents needed are a formal application or request letter, your full name, registration number, and course details, a copy of the nursing license if it is applicable, a copy of your degree or diploma certificate, a government-issued ID like a passport, CNIC, evidence of payment of transcript fees if needed, and other forms required by the institution or authority. Your documents are clear, legible, and current so that they won’t be rejected. Submitting the transcript request After preparing your documents, you can go ahead and submit your request for a transcript to the relevant office. Submission is usually possible in person, by post, or online if the institution provides electronic services. When doing it in person, it is advisable to visit the office to confirm working hours and whether an appointment is required. If you are mailing, using a trusty courier service and attaching all required documents is advisable. When applying online, ensure you are obedient to instructions and upload good-quality scans of requested documents. It is always prudent to retain a copy of your application and any receipts for payment for your reference. Paying the required fees It is common for most institutions to have a processing fee for transcript issuance, which can differ based on the number of copies, the location—local or international—and the urgency level, regular or urgent submission. Paying the appropriate fee through the designated payment mechanism, bank drafts, online payment systems, or cash at the accounts office, is crucial in order to prevent delays. Following up on your request After making your request, it’s essential to follow up, particularly if you have a deadline to achieve. Call the concerned office via phone or email to inquire about the status of your transcript request. Institutions may offer a tracking number or portal to track progress. Be polite in your interaction and always mention your application number or receipt number so the staff can easily find your request. Receiving and verifying your transcript You will receive your transcript once it is prepared, either picking it up from the issuing authority or having it posted to your preferred address. In some instances, the transcript may only be forwarded straight to the licensing board or the school, since there are institutions that would not accept transcripts that have gone through the applicant’s hands. Upon receiving the transcript, it is essential to verify that your name is spelled correctly, all course details and grades are accurate, the document is signed and stamped by the appropriate authority, and the envelope is sealed and marked “official” if required by the receiving organization. If you notice any mistakes, notify the issuing authority at once for rectification, as even small differences can create problems with your application or assessment. Conclusion Obtaining a nursing transcript certificate is a vital step towards career progression for nurses either within the locality or overseas. Even though the procedure will differ from your institution and country, it usually includes determining the issuing authority, getting the documents ready, submitting the application, paying required fees, following up, and ensuring that your transcript is accurate. Being detailed, proactive, and organized will ensure a seamless process. With your nursing transcript certificate in hand, you will be more capable of seeking licensure, further education, or professional opportunities that suit your objectives.
What You Can Do With A Practical Nursing Certificate Career Opportunities And Beyond

Obtaining a practical nursing (PN) certificate is a thrilling move toward a fulfilling and meaningful career in healthcare. A Practical Nursing certificate offers a range of opportunities for individuals with a passion for assisting others, a desire to make a positive impact on people’s lives, and a willingness to work in a dynamic healthcare environment. Regardless of whether you are starting your career in nursing or seeking a change, becoming a practical nurse offers a path to a secure, rewarding, and much-needed career. A certificate program in practical nursing provides you with the necessary knowledge, clinical competency, and practical training to deliver direct patient care with the guidance of registered nurses (RNs) and physicians. These programs focus on fundamental nursing skills, including patient care, medication administration, vital signs monitoring, wound care, and effective communication. The need for practical nurses remains strong, fueled by an aging population, high rates of chronic disease, and a general requirement for qualified healthcare providers in all types of settings, from hospitals and clinics to long-term care facilities and home healthcare. But what can you do with a Practical Nursing certificate? Students often ask how far this certification will take them, what they can do with their careers, and how they can use it as a starting point to establish a successful and rewarding career. Become a licensed practical nurse (LPN) The most direct and common outcome of completing a Practical Nursing program is becoming a Licensed Practical Nurse (LPN), also known in some states as a Licensed Vocational Nurse (LVN). As an LPN, you’ll work under the supervision of Registered Nurses (RNs) and physicians, providing essential nursing care such as: Monitoring patients’ health by taking vital signs (blood pressure, pulse, respiration, temperature). Administering prescribed medications and injections. Helping patients with activities of daily living like bathing, dressing, and eating. Performing basic wound care and dressing. Notifying the healthcare team about changes in a patient’s condition. LPNs are involved in ensuring that patients receive quality care, providing emotional support as well as physical support throughout the healthcare process. Work in a variety of healthcare settings A practical nursing certificate enables you to work in several environments including: Hospitals: LPNs assist those recuperating from severe illness or post-surgery recovery, and monitor vitals. Long-term care facilities and nursing homes: LPNs look after the aging members of society, assist them with mobility, and monitor chronic illnesses. Home healthcare: LPNs are the ones who visit homes to provide one-on-one care and build good relations with the families and patients. Outpatient care facilities: Those LPNs attached to outpatient care facilities assist with the intake of patients, minimally invasive procedures, immunizations, and health teaching in clinics and doctor’s offices. Rehabilitation center: The LPN helps a patient in overcoming a particular disease, injury, or surgery and return to their independent status. Specialize in a niche area of care LPNs may decide to specialize in the following: Pediatrics: Caring for children in clinics, hospitals, or pediatric long-term care facilities. Geriatrics: Providing care to older patients with age-related health concerns. Hospice and palliative care: Caring for patients with life-limiting illnesses, with an emphasis on comfort and quality of life. Maternity and obstetrics: Assisting in prenatal care, labor and delivery support, and postpartum care. Surgical nursing: Preparing patients and assisting patients through surgery. These specializations not only enable LPNs to work in areas of their choice but can even lead to better-paying positions and leadership responsibilities in their desired field. Advance your career through further education Having a Practical Nursing certificate can also serve as a stepping block for career advancement in nursing. LPNs opt to carry on their education by taking LPN-to-RN bridge programs or a Bachelor of Science in Nursing (BSN). This route enables LPNs to: Have greater responsibility and autonomy as a registered nurse. Enhance their earning power. Have more career options available to them, such as leadership, education, and specialty nursing positions. LPNs sometimes advance to become Nurse Practitioners (NPs) or seek advanced degrees in nursing education or health administration. Opportunities for leadership and mentoring Veteran LPNs tend to assume leadership positions in their setting. They can be Charge Nurses, responsible for a group of nursing assistants and other LPNs. They may take new nurses as their mentees, helping train and mentor them in their transition into the profession. This way, LPNs can have a significant influence on the culture of their work environment and the standard of patient care. Conclusion Your Practical Nursing certificate gives you a solid foundation for a future filled with possibilities whether you decide to serve as a frontline caregiver in a hospital setting, specializing in a specific area of nursing, go on to earn your RN or venture into entrepreneurial pursuits. The need for skilled and caring nurses increases, and with your education and commitment, you can positively impact the lives of patients, families, and communities. By becoming a practical nurse, you’re not merely earning a credential — you’re entering an honored profession with a commitment to care, compassion, and a lifetime of learning. The opportunities are as vast as your imagination, and through perseverance, you can create a career that’s both personally rewarding and professionally satisfying.
What Is Nursing Assistant Training?

The healthcare sector is one of the fastest-growing industries in the world, and it needs a large variety of professionals to cater to the various needs of patients. Of these professionals, nursing assistants, also known as certified nursing assistants (CNAs), nurse aides, or patient care assistants, are essential. These professionals offer basic care and assistance to patients under the guidance of registered nurses (RNs) or licensed practical nurses (LPNs). Since nursing assistants spend a lot of time with patients and have a direct influence on their comfort and welfare, adequate training is necessary and compulsory in the majority of nations. Nursing assistant training provides people with the fundamental knowledge and skill set to provide empathetic, efficient care. The training also teaches students how to help with activities of daily living like bathing, dressing, feeding, mobility, and vital sign observation. In addition to that, it gives a tremendous sense of ethics, patient privacy, and how to communicate with the techniques in a clinical practice. This preparation is usually for individuals who aim to pursue careers in nursing or healthcare, a career opportunity for itself as well as a building block to advance in more responsibilities. As the demand for geriatric care, long-term care, and rehabilitation increases, the demand for properly trained nursing assistants also keeps on growing. Nursing assistant training is a formal program that provides preparation for the practical and psychological challenges of the healthcare setting. What does nursing assistant training include? Nursing assistant training programs are generally provided by community colleges, vocational schools, hospitals, and even high schools in certain places. The curriculum is generally segregated into theoretical teaching and practical clinical training. The theoretical sessions include anatomy and physiology, infection control, nutrition, patient’s rights, and the legal and ethical obligation of a nursing assistant. Students are taught how to identify patient condition changes and how to report them, and also about maintaining hygienic standards so that no infection spreads. Also necessary is hands-on training. The students learn how to do the necessary chores of turning and repositioning patients, moving patients between beds and wheelchairs, toileting, and operating medical devices such as blood pressure cuffs or thermometers. They also learn to communicate with the patients, who are often elderly, confused, or chronically ill. At the culmination of training, students should possess competence in both interpersonal interaction and technical skills. Nursing assistant training varies in time by location or program design, but it mostly takes between 4 and 12 weeks. Duration and format of training programs Some specialized programs can take just a matter of weeks to complete, although part-time and evening classes would last several months. The majority of programs involve 75 to 150 hours of blended classroom education and clinical training, depending on the local health authority or certification board requirements. For instance, in the United States, the federal minimum for CNA training is 75 hours with a minimum of 16 hours of supervised clinical practice. But numerous states provide more than this minimum to equip students with more than just the minimum to meet the harsh realities of patient care. Training can be offered in various formats—classroom settings (traditional), online modules (for the theoretical aspects), and on-site clinical training in healthcare centers like nursing homes, hospitals, or rehabilitation centers. The flexibility of format accommodates students with other commitments, like a job or family, to transition into a career in the healthcare field without giving up their existing commitments. Skills and knowledge acquired Nursing assistant education encompasses a wide range of skills that equip students for real-world challenges in clinical settings. These include technical, interpersonal, and emotional abilities. Technically, students learn to take vital signs, aid patients with hygiene, handle bed linens, assist patients with mobility, and identify signs of distress or deterioration. Communication is also an essential aspect of the training. Nursing assistants need to be able to communicate professionally with patients, families, nurses, and physicians. They are taught to support patients emotionally, to advocate for patients during difficult conversations, and to cope with patients who might have cognitive impairments like dementia. Another important area is cultural competence. Because healthcare facilities are attended to by individuals from a variety of backgrounds, nursing assistants are taught to be respectful of cultural differences, religious beliefs, and personal preferences, all of which are important to providing patient-centered care. Trainees are also taught workplace safety, emergency response, and how to deal with incidents such as patient falls, bed sores, or behavioral problems in a professional, calm manner. Importance of nursing assistant training in healthcare Nursing assistant training is crucial to the functioning of the healthcare system as a whole. CNAs are the frontline workers who spend the most time with patients. They often are the first to see medical complications or emotional distress. Their input and communication with the nursing staff can greatly influence patient outcomes. Additionally, trained nursing assistants assist in offloading the work of nurses and doctors so that they can specialize in more complex medical interventions. This task delegation enables the health facility to be well-organized and ensures patients receive uninterrupted and empathetic care. Proper training also guarantees nursing assistants treat patients with respect and dignity, something crucial in patient and family trust and morale. Where compassion and technical proficiency are required to go hand in hand, well-educated nursing assistants are irreplaceable. Conclusion The training of nursing assistants is a building block of the health care system, providing individuals with the knowledge, skills, and moral awareness necessary to deliver critical patient care. Through the acquisition of technical skills and patient communication, certification, and clinical experience, the process of becoming a certified nursing assistant is demanding but rewarding. As the need for healthcare services will continue to increase, especially in the face of aging populations and greater emphasis on long-term care, nursing assistants will continue to be essential in providing patients with high-quality, respectful, and consistent care. For others, nursing assistant training is not only the start of a rewarding profession but also the gateway to further positions
Financial Planning For Nursing Students

Nursing is one of the most rewarding and secure careers, providing a variety of career paths and the opportunity to leave a lasting impression on individuals’ lives. Nevertheless, becoming a nurse can be costly. Fees for tuition, textbooks, laboratory supplies, uniforms, clinical materials, transportation, and living expenses soon mount up, frequently placing nursing students under financial pressure. A lot of students also cut back on working hours or quit working entirely during stressful clinical rotations or tests, which makes budgeting all that more challenging. Financial planning isn’t merely a good idea—it’s necessary. Learning effective financial habits from the beginning can assist nursing students in being better money managers, lowering stress levels, and graduating with less debt. Financial planning equips students with the skills to make prudent decisions regarding borrowing, spending, saving, and investing in the future. Financial planning enables them to prioritize wants over needs and prepare for emergencies like vehicle repair or healthcare bills. Financial planning also saves one from psychological stress caused due to money that may otherwise compromise academic performance. Creating a realistic budget The basis of any good financial plan is a realistic and comprehensive budget. Nursing students can begin by monitoring their income (from summer jobs, scholarships, grants, family aid, etc.) and creating a comprehensive list of expenses. These expenses can be tuition fees, rent, food, transportation, school materials, medical insurance, and personal expenditures. Being realistic is important. Very tight budgets create frustration and subsequent overspending. It’s also necessary to review the budget periodically and make changes based on a change in income or expenses, like getting a scholarship or a new job. Understanding and managing student loans Nursing students often use student loans to finance their education. Although loans can be helpful financially, they can create long-term debt if not managed properly. It is essential to know the terms and conditions of student loans—federal or private. Students should be aware of the interest rates, grace periods, repayment terms, and total borrowed amount. Federal student loans should be used whenever possible because they tend to have lower interest rates and more lenient repayment terms. Nursing students who intend to work in underserved areas or government-funded healthcare facilities can be eligible for such forgiveness programs upon graduation. To pay loans effectively, students ought to borrow just as much as they need. Even if the loan is sanctioned for more money, borrowing less saves future repayment stress. Paying small interest during school, if feasible, can also decrease the overall repayment burden. Saving strategies for students Even on a tight budget, saving remains possible—and necessary. Creating an emergency fund, even a small one beginning with a few hundred dollars, can serve as a cushion for unforeseen expenses. This may keep students from using high-interest credit cards in the event of car repairs or medical expenses. Students might think about opening a high-yield savings account or a student bank account with no maintenance fee. Setting up automatic transfers helps in building the habit of saving. Also important is saving money on a frugal lifestyle. Purchasing used textbooks, carpooling to class, preparing meals at home, using student discounts, and sharing supplies with classmates can all result in substantial savings in the long run. Each dollar saved is a dollar that can be put toward a more necessary cost or applied to eliminate debt. Balancing school and part-time work Most nursing students work part-time to finance themselves. But it’s crucial to find the right balance. Excessive work can result in burnout, poor academic performance, and health issues, particularly during stressful clinical rotations or exam times. The ideal jobs for nursing students are flexible, low-stress, and ideally healthcare-related. Jobs like being a certified nursing assistant (CNA), medical scribe, or front desk clerk in a clinic can generate income as well as provide pertinent experience. On-campus employment also tends to be more flexible with student schedules. Students should determine how many hours they can maintain per week without sacrificing their coursework. With a time management schedule that includes class, study time, clinical, and work, it is possible to avoid overload. Making use of financial tools and resources There are also several different financial resources and tools available to assist nursing students in remaining on track. Universities also tend to offer financial counseling and budgeting, debt management, and scholarship application workshops. Taking part in these sessions can improve financial literacy and provide students with insider advice and lesser-known sources of funding. Credit unions and student-friendly banks might also provide financial education programs and one-on-one advice. It’s worth meeting with a financial advisor, particularly at key times such as applying for aid or graduation. Planning for life after graduation Financial planning must carry over past nursing school. When students graduate and begin earning a salary, it’s essential to move into longer-term financial strategies. This would involve developing a post-graduation budget, beginning to pay back loans, establishing a stronger emergency fund, and saving for retirement through employer-sponsored plans. The employment offers should be carefully considered by new nurses. Health benefits, loan repayment bonuses, sign-on bonuses, relocation expenses, etc., should not be overlooked compared to base salary. Developing a financial plan during the first year post-graduation can keep one from acting on impulse and promote saving and investing from an early stage of one’s working life. Conclusion Financial planning is an important skill for nursing students, one that serves them both in academic achievement and overall well-being. With the workload of a demanding program, students cannot afford to be burdened by financial concerns. By being taught to budget, use loans responsibly, seek aid, save, and juggle work with school, nursing students can lay the groundwork for financial success both in school and after. The path to becoming a nurse takes more than learning clinical skills—it takes a proactive attitude towards personal finance. Students who take the time to plan and make smart financial choices now will graduate with more confidence, less debt, and more autonomy to follow their career aspirations without the weight of financial uncertainty.
Technological Advancements In Nursing

The profession of nursing, based on empathy and hands-on care, has been revolutionized in the past few decades—primarily because of fast-paced technological progress. In a world characterized by digitalization and innovation, technology is no longer an ancillary device; it is now deeply integrated into the healthcare delivery process. From electronic health records (EHRs) to smart IV pumps and artificial intelligence (AI) decision support, nursing has come a long way to adapt to the needs of today’s healthcare settings. Not only are these innovations enhancing patient care but also transforming the way nurses practice. They are facilitating improved care team communication, minimizing medication errors, better supporting clinical decision-making, and enabling nurses to focus more on patient time versus paperwork. Advances like wearable health trackers, mobile health apps, telehealth solutions, and robotic aids are empowering nurses to provide more effective, individualized, and anticipatory care. For the nurse of today, computer literacy is as important as medical expertise. Though there may be a learning curve in adopting such tools, particularly for experienced professionals trained in traditional ways, the advantages far compensate for the pains of change. Nurses who adopt technology are discovering new opportunities to enhance results, increase workflow efficiency, and help foster a more data-driven healthcare environment. Electronic health records (EHRs): streamlining patient data The move away from paper-based records to Electronic Health Records (EHRs) has transformed the way nurses document, access, and manage patient information. EHRs provide an integrated, up-to-date system for monitoring patient histories, laboratory results, medication administration, and treatment plans. For nurses, EHRs enhance accuracy and eliminate redundancy. Rather than typing out long notes, nurses may employ templates, voice-to-text functionality, or touch-screen entries to capture data quickly. EHRs also reduce errors related to poor handwriting or missing files, providing improved continuity of care between departments and providers. In addition, the inclusion of decision-support tools within EHR systems notifies nurses of possible drug interactions, allergy risks, and abnormal laboratory results, supporting safer clinical decisions. Yet, consistent training is necessary to allow nurses to use these systems to the fullest and prevent documentation fatigue. Telehealth and remote nursing care Telehealth is now among the most revolutionary developments in nursing, particularly since the COVID-19 pandemic pushed it to gain rapid acceptance. Telehealth allows nurses to deliver care remotely through video conferencing, phone calls, and digital channels, helping patients who reside in rural settings, have mobility issues, or need chronic disease management. Remote monitoring devices, including blood pressure cuffs, glucometers, and pulse oximeters linked to mobile apps, enable nurses to monitor patient vitals remotely and take early action when abnormalities are noted. Nurses are instrumental in telehealth by: Performing virtual exams Teaching patients how to use devices Facilitating follow-up care Encouraging treatment plan adherence Telehealth increases access and convenience, but it also demands that nurses build excellent communication skills and technology expertise to sustain high-quality care through virtual mediums. Smart IV pumps and medication administration technology Medication errors are one of the most threatening patient care hazards. Smart infusion pumps, barcode scan systems, and automatic dispensing cabinets (ADCs) are technologies aimed at improving medication safety. Smart IV pumps rely on drug libraries and assignable dose limits to avoid infusion errors. Nurses can enter specific infusion parameters and be warned about potentially unsafe doses or rates. Barcode medication administration (BCMA) requires scanning the patient’s wristband and the barcode of the medication before administration. The system guarantees the “five rights” of medication administration: right patient, right drug, right dose, right route, and right time. These technologies minimize the room for error and enable nurses to concentrate more on patient monitoring instead of manual cross-checking, which eventually results in safer and more efficient care. Artificial intelligence (AI) and predictive analytics Artificial intelligence (AI) is being incorporated more broadly into nursing practices, most notably through predictive analytics to enable early intervention. Large datasets are scanned by AI algorithms for patterns and possible signals of health decline before it becomes serious. For instance, AI-based solutions can notify nurses of patients who are at risk of sepsis, pressure ulcers, or hospital readmission. This enables nurses to stage interventions, implement preventive care, and coordinate timely interventions. AI also helps in staffing models, patient triage, and even automating documentation. While AI cannot replace human judgment, it complements the nurse’s role by offering actionable information and evidence-based decision support. Wearable health devices Wearable technology, including smartwatches, fitness trackers, and biosensors, is becoming more popular in nursing practice. Wearables monitor vital signs, activity, sleep, and even hydration or blood glucose levels continuously. For nurses, wearables give real-time feedback to aid in the early detection of complications. Wearable sensors in post-operative or chronic care patients can alert care teams when abnormalities are present, preventing hospital readmission and enhancing patient independence. Wearables also increase patient engagement. If patients can view their data, they are more likely to stick to care plans. Nurses then become critical in interpreting that data, answering questions, and modifying care as needed. Robotics and automation in nursing tasks As much as the notion of robots in nursing sounds like something from a science fiction movie, it is already in the making in most hospitals. Robotic systems are being employed to aid in repetitive or physically demanding procedures like: Delivery of medications or meals to patient rooms Transportation of medical supplies Support with patient mobility and lifting These devices allow nurses to spend more time on more complicated, patient-focused activities, decreasing physical fatigue and enhancing job satisfaction. In addition, robotic simulation devices are also applied in nursing education to educate students on clinical situations, enhancing readiness and decision-making skills before exposure to actual environments. Simulation and virtual reality in nursing education Technological innovation is not only affecting clinical practice—it’s also changing nursing education. Simulation classrooms, which feature high-fidelity manikins and virtual reality (VR) systems, provide interactive, risk-free environments for nurses and students to hone skills. Such situations as cardiac arrest, birth, wound treatment, and treatment of infectious diseases can be simulated in controlled environments. VR devices also enable nurses to empathize
